Targeted drug therapy in haematology refers to treatments that specifically attack cancer cells or abnormal blood cells by focusing on particular molecules (targets) involved in their growth, survival, or signaling rather than broadly killing all rapidly dividing cells like traditional chemotherapy. The drug is designed to block, inhibit, or destroy cells with that target, sparing most normal cells.
Common types of targeted therapy in hematology includes Tyrosine kinase inhibitors (TKIs),Monoclonal antibodies, Antibody–drug conjugates, Small molecule inhibitors, Epigenetic modifiers. The Advantages of doing targeted drug therapy is more specific than chemotherapy ,often fewer systemic side effects, Can be taken orally (many agents),Highly effective when the target is present.
IMMUNOTHERAPY IN HEMATOLOGY:
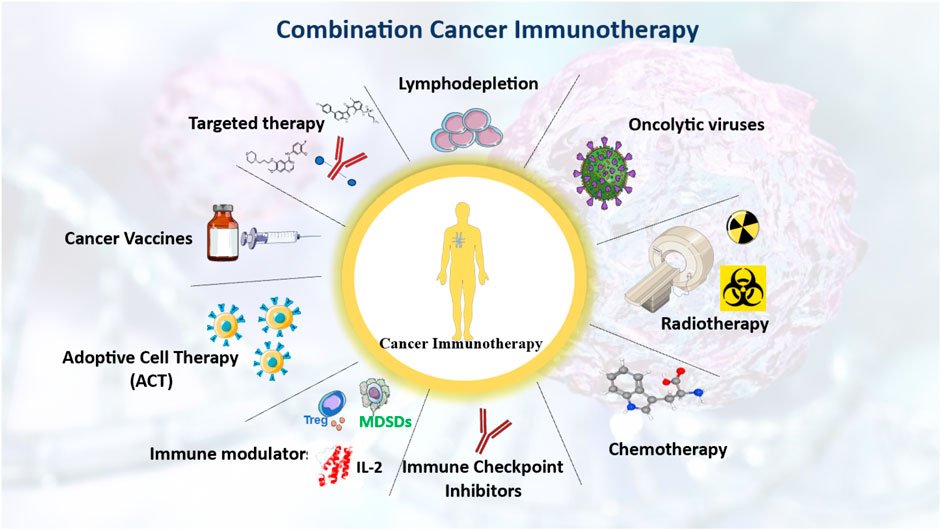
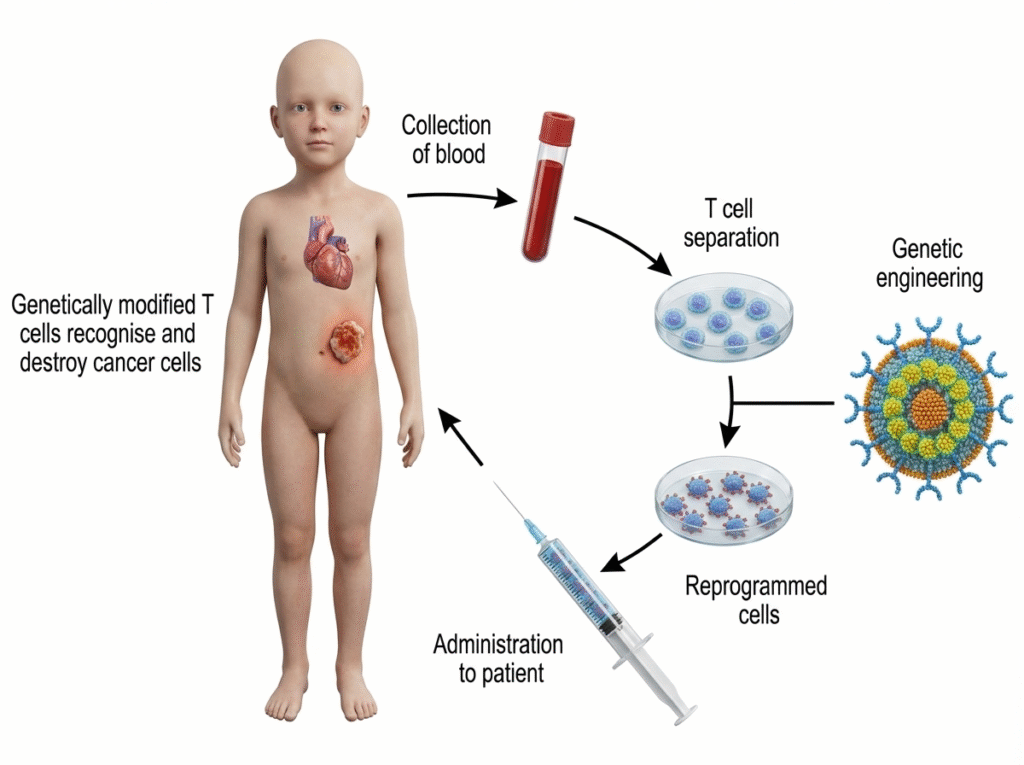
Immunotherapy in hematology is a treatment approach that uses the patient’s own immune system (or immune-based drugs) to recognize, target, and destroy abnormal blood cells or blood cancers.
Instead of directly killing cancer cells like chemotherapy, immunotherapy:
- Enhances immune response
- Removes immune checkpoints
- Directs immune cells to attack cancer cells
Types of immunotherapy in hematology includes Monoclonal antibodies, Immune checkpoint inhibitors, CAR-T cell therapy, Bispecific T-cell engagers (BiTEs),Immunomodulatory drugs (IMiDs), Cytokine therapy. The Advantages of doing Immunotherapy in hematology is highly specific, can produce long-lasting

